
|
Читайте также: |
Meningococcal Infection
Epidemiology
| Spread | All over the world | ||||
| Dominating serotypes | |||||
|
| ||||
| Source of the infection | Symptomatic patients and carriers (up to 2000 carriers per 1 symptomatic) | ||||
| Way of transmission | Respiratory | ||||
| Morbidity | 41,19 per 100 000 (Ukraine 1998y.) | ||||
| Epidemic cycle | 8-30 years | ||||
| Contagiousness | 10-15% in non-vaccinated | ||||
| Seasonal morbidity | January-March | ||||
| Age distribution |
| ||||
| Mortality (Ukraine 1998y.) |
| ||||
| Carriage rate | 5-10% | ||||
| Carriage rate during epidemics in closed populations | 100% |
• Serogroups A, B, C, W135, X, Y, and Z – by capsular polysaccharide antigen.
• Most strains causing meningococcal disease have the of groups A, B, or C.
Higher risk of meningococcal infection:
• Freshmen college students, especially living in dormitories
• Viral infections (facilitate invasion)
• Smoking and smoke exposure
• Crowded living conditions
• Underlying chronic diseases
• Low socioeconomic status
Microbiology:
N.meningitidis:
• Gram-negative
• Intra- and extracellular bacteria
• not stable to outer influence
• Serogroups А and В typically give generalized infections
• Serogroup A is responsible for epidemics
• Can autolyse – endotoxin is released
•

Development of meningococcemia:
Absence of antimeningococcal antibody
↓
Bacteriemia
↓
Interaction with phagocytes + adhesion to endothelial cells
↓
Complement system activation + attachment of white blood cells to endothelium
↓
Production of multiple proinflammatory cytokines (TNFa, IL-1ß, IL-6, and IL-8) + activation of both the extrinsic and intrinsic pathways of coagulation
↓
Capillary leak and disseminated intravascular coagulopathy (DIC)
↓
Leukocyte-rich fibrin clots in small vessels
↓
Focal hemorrhage and necrosis in any organ system
↓
Heart, CNS, skin, mucous and serous membranes, and adrenals are affected in most fatal cases
↓
Multiple organ system failure, septic shock, and sometimes death
↓
Fatal cases typically have higher concentrations of TNFa and ILs
↓
TNFa and ILs levels decrease rapidly once antibiotics are given
↓
Fatality risk is higher in children capable of strong immune response
Meningococcal survival is enhanced by:
• Polysaccharide capsule, which helps resist phagocytic killing
• Iron scavenging system that can use host transferrin and lactoferrin
Predisposition:
• Complement component deficiencies → increased susceptibility to and recurrent cases of meningococcal infections
• Immunoglobulin G2 subclass deficiency → recurrent meningococcemia
• Hereditary properdin deficiency → predisposition to meningococcal disease
Natural immunity against N. meningitides:
• After repeated colonization with different serogroups or serotypes
• From gastrointestinal colonization with enteric bacteria that express cross-reactive antigens
• Infants also have high carriage rates of the unencapsulated, nonpathogenic neisserial strain, N. lactamica → immunity against meningococci
• Protective effects of maternal IgG during only the first 3 months of life
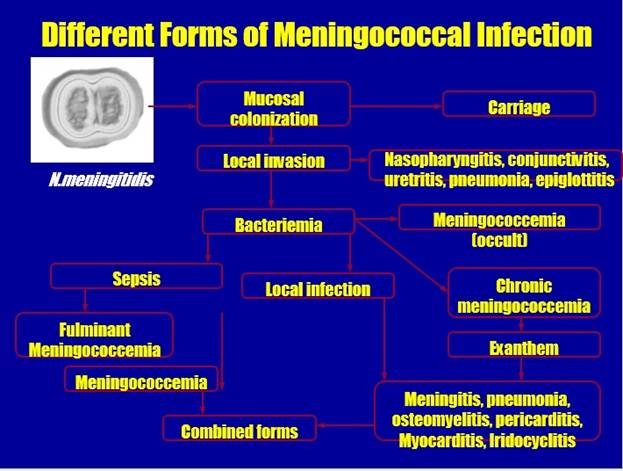
Classification of meningococcal infection:
| Form | Localized Generalized Rare forms |
| Course | Acute Subacute Fulminant Recurrent |
| Severity | Mild Moderate Severe |
Forms of meningococcal infection:
| Localized forms: Carriage Nasopharyngitis Generalized forms: Meningococcemia Meningitis Meningoencephalitis Meningococcemia with meningitis | Rare forms: Endocarditis Arthritis Iridocyclitis Pneumonia Urethritis Otitis Conjunctivitis |
Meningococcemia (meningococcal sepsis):
ü Accounts for 15-20% of all invasive cases of meningococcal infection.
ü Mortality is 20 - 40%.
ü Superacute meningococcal sepsis develops in 10-20% of cases.
ü Mortality from Superacute meningococcal sepsis is over 90%.
Clinical Presentations
| ||
|
Meningococcal rash (Loclization):
Hemorrhagic rash with uneven borders and central necrosis, first appear on lower extremities and buttocks
Waterhouse-Friderichsen syndrome:
• In fulminant cases, the disease progresses rapidly over hours to septic shock characterized by hypotension, DIC, acidosis, adrenal hemorrhage, renal failure, myocardial failure, and coma.
Criteria of severity: (Damroshe Scale (1966)
Every index has 1 point.
3 points: case fatality rate is 85,7%,
≥ 4 points: 100%
Criteria of severity:(Niklasson Scale (1971)
Every index has 1 point.
≥ 4 points: case fatality rate is 100%
Criteria of severity: (Glasgow Meningococcal Septicemia Scale (1991)
| Systolic pressure < 75 mm.Hg. (under 4 years), < 85 mm.Hg. (older 4 years) | 3 points |
| Gradient of skin-rectal temperature >3°С | 3 points |
| Glasgow Coma Scale < 8 points | 3 points |
| . “Every hour” previous worsening of condition | 2 points |
| Absence of Meningeal signs | 2 points |
| Spread hemorrhagic rash with large elements | 1 point |
| Base deficit (pH>8,0) | 1 point |
8 points– fatality rate 73%, 10 points – 87,5%, 12 and more – 100%
Differential diagnosis:
| Scarlet fever Measles Rubella Exanthema subitum Dengue Fever Gonococcal infection Influenza Mycoplasma infections Rocky Mountain Spotted Fever | Streptococcal Group A & B infections Thrombocytopenic Purpura Ebola Virus Enterovirus Infective Endocarditis Malaria Drug reactions Poisonings |
Diseases with hemorrhagic rash:
• Neisseria meningitidis
• Haemophilus influenzae
• Streptococcus pneumoniae
• Neisseria gonorrhoeae
Diagnosis in children with fever and hemorrhagic rash (Baker R.C. et al, Pediatrics, 1989):
| Bacterial sepsis | 39 (12,2%) |
| Neisseria meningitidis | 26 (8,2%) |
| Haemophilus influenzae type b | 9 (2,8%) |
| Streptococcus pneumoniae | 2 (0,6%) |
| Staphylococcus aureus | 2 (0,6%) |
| Other bacterial infections | 68 (21.3%) |
| Bowel infection caused by Escherichia coli | 3 (0,9%) |
| Streptococcal tonsillitis | 23 (7,2%) |
| M. pneumoniae pneumonia | 1 (0,3%) |
| Pneumonia of unknown etiology | 11 (3.4%) |
| Acute otitis media | 30 (9,4%) |
| Ricketsiosis | 1 (0,3%) |
| Viral infections | 195 (61,1%) |
| Enteroviral infection | 9 (2,8%) |
| Aseptic meningitis | 16 (5%) |
| Adenoviral infection | 1 (0,3%) |
| RS-infection | 12 (3,8%) |
| Human methapneumovirus | 11 (3,4%) |
| Rotavirus | 1 (0,3%) |
| HHV-6 (exanthema subitum) | 1 (0,3%) |
| Probable viral infection | 144 (45,1%) |
| Other causes | 25 (7,9%) |
| Hemorrhagic vasculitis | 2 (0,6%) |
| Kawasaki disease | 1 (0,3%) |
| Thrombocytopenic purpura | 1 (0,3%) |
| Vaccination reaction | 3 (0.9%) |
| Acute leukemia | 2 (0,6%) |
| Febrile seizures | 5 (1,6%) |
| Partially treated meningitis | 2 (0,6%) |
| Partially treated septicemia | 2 (0,6%) |
| Exudative tonsillitis | 2 (0,6%) |
| Reaction to ampicillin | 1 (0,3%) |
| Unknown | 4 (1,3%) |
Occult meningococcemia:
• Fever with or without associated symptoms that suggest minor viral infections
• Resolution may occur without antibiotics, but some cases will develop meningitis
Chronic meningococcemia:
Rare form: Intermittent Bacteriemia illness that lasts from at least one week to as long as several months
– Intermittent fever, with afebrile periods ranging from 2-10 days, during which the patient seems entirely healthy → febrile periods occur more frequently, fever may become continuous;
– Headache, arthritis can develop;
– Eventually, skin hemorrhages or signs of meningitis appears during a febrile episode;
– Blood cultures may initially be sterile.
Дата добавления: 2015-10-29; просмотров: 148 | Нарушение авторских прав
| <== предыдущая страница | | | следующая страница ==> |
| The Anatomy of the Heart | | | Програма літньої організаційно-виховної практики |