
Читайте также:
|
In many parts of the body, collagen fibers are organized in a parallel array, forming collagen bundles.
Reticular fibers are extremely thin, with a diameter between 0.5 and 2 μm. They form an extensive network in certain organs. They are not visible in hematoxylin and eosin preparations but can be easily stained black by impregnation with silver salts. Because of their affinity for silver salts, they are called argyrophilic. Immunocytochemical evidence reveals that reticular fibers are composed mainly of collagen type III in association with other types of collagen, glycoproteins, and proteoglycans.
Reticular fibers are particularly abundant in smooth muscle, endoneurium, and the framework of hematopoietic organs and constitute a network around the cell of parenchymal organs (liver, kidney, endocrine glands). During embryogenesis, inflammatory processes, and wound healing, most connective tissues have an abundance of reticular fibers, but these are subsequently replaced by regular collagen fibers.
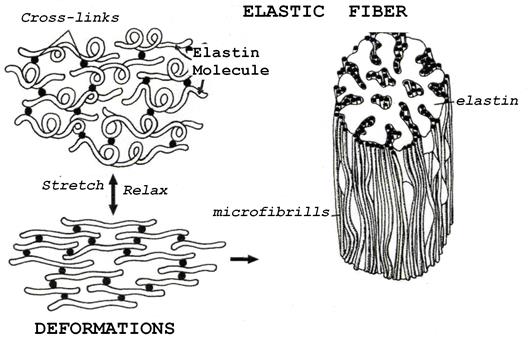
Elastic Fiber System is composed of three types of fibers – oxytalan, elaunin, and elastic. The structure of the elastic fiber develops through three successive stages that can be observed in both embryonic and adult tissue. In the initial stages, the fiber is composed of a bundle of thin, glycoprotein (fibrillin) -containing microfibrils. - oxytalan fibers. In the next stage of development, an irregular deposition of the protein elastin appears between the oxytalan fibers forming the elaunin fibers. During the third stage, elastin gradually accumulates until it occupies the center of the fiber bundles, which are further surrounded by a thin sheath of microfibrils. These are the elastic fibers, the most numerous component of the elastic fiber system.

Elastin is the amorphous rubber-like glycoprotein that predominates in the mature fibers. It is produced by fibroblasts in the skin and tendon and by smooth muscle cells in the large blood vessels. Elastin also occurs in a nonfibrillar form as fenestrated membranes (elastic laminae) present in the walls of some blood vessels.
CELLS
Some cells of connective tissue, such as fibroblasts and adipose cells, are produced locally and remain there (residents); others, such as leukocytes, come from other territories and can be transient inhabitants of connective tissue (immigrants).
Cells of the connective tissue interact, creating complex mechanisms that help defend the organism from invasion.
FIBROBLASTS. The fibroblast is the cell most commonly found in connective tissue. It is responsible for the synthesis of fibers and amorphous intercellular substance. Two stages of activity – active and quiescent in this cell are observed. The cell with intense synthetic activity – fibroblast - is morphologically distinct from the quiescent cell - fibrocyte that is found scattered within the matrix it has already synthesized.

 Fibroblast and fibrocyte
Fibroblast and fibrocyte
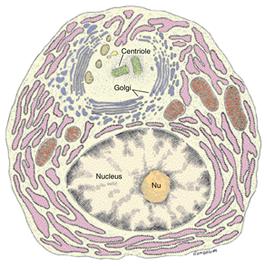
The active fibroblast has an abundant and irregularly branched cytoplasm. Its nucleus is ovoid, large, and pale-staining, with fine chromatin and a prominent nucleolus. The cytoplasm is rich in rough endoplasmic reticulum, and the Golgi complex is well developed.
The fibrocyte, a smaller cell than the fibroblast, tends to be spindle-shaped. It has fewer processes than the fibroblast; a smaller, darker, elongated nucleus; an acidophilic cytoplasm; and a small amount of RER.
The myofibroblast is observed during wound healing. These cells have the morphologic characteristics of a fibroblast, but contain increased amounts of actin microfilaments and myosin. Their activity is responsible for wound closure following tissue injury, a process called wound contraction.
Fibroblasts synthesize:
· collagen, reticular and elastic fibers,
· the glycosaminoglycans and glycoproteins of the amorphous intercellular substance.
MACROPHAGES. These cells are characterized by their phagocytic capacity.
Macrophages derive from HSC through the stage of monocytes that circulate in the blood. Then these cells migrate into the connective tissue where they mature and are called macrophages (or, histiocytes).
Macrophages, which are distributed throughout the body, constitute the mononuclear phagocyte system. In certain organs, macrophages have special names, e.g., Kupffer cells in the liver, microglial cells in the central nervous system, fibroclasts, chondroclasts, and osteoclasts in connective tissues etc.
To be classified as components of this system, phagocytes must:
• 1) be derived from bone marrow stem cells;
• 2) have characteristic morphologic features;
• 3) exhibit relatively intense phagocytic activity mediated by immunoglobulins or serum complement.
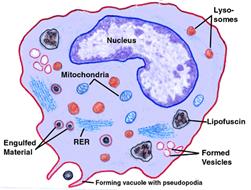
Morphological features of macrophages:
• an irregular surface with pleats, protrusions, and indentations – a morphological expression of their active phagocytic activity;
• they generally have many lysosomes, phagolysosomes;
• macrophages measure between 10 and 30 μm and usually have an oval or kidney-shaped nucleus located eccentrically.
Functions:
I. The major functions of macrophages are the ingestion of particles and their digestion by the lysosomes. Engulfment is performed by surrounding the particle with thin extensions of the cell surface that ultimately fuse, isolating the particle within a phagocytic vacuole. Next, lysosomes fuse with the phagocytic vacuole and digest the contents.
Fig.5.
II. In addition to this function, macrophages participate in the immune system of the body. Macrophage takes up an antigen, processes it (partially digests foreign proteins in lysosomes) and presents antigen to lymphocytes and thereby activating them. Thus, macrophages are referred as antigen-presenting cells (Fig.6).
 Fig.6.
Fig.6.
III. Macrophages secrete of an impressive array of substances that participate in defensive and reparative functions, such as interleukin-1, stimulating leukocytes’ activities; factors, stimulating differentiation of T- and B-lymphocytes; cytolytic antitumor factors, and growth factors, stimulating formation of macrophages and fibroblasts.
IV. Macrophages also participate in the destruction of aged erythrocytes, and iron and fat metabolism.
MAST CELLS. The principal function of mast cells is the storage of chemical mediators of the inflammatory response. Mast cells are oval to round connective tissue cells, 20-30 μm in diameter, whose cytoplasm is filled with basophilic granules. The rather small and spherical nucleus is centrally situated; it is frequently obscured by the cytoplasmic granules.
Their interior is heterogeneous in appearance, with a prominent scroll-like substructure. Mast cell granules are metachromatic because of their content of GAG (heparin or chondroitin sulfate) containing:
• heparin is a substance with anticoagulant activity.
• histamine causes contraction of smooth muscle (mainly of the bronchioles), dilate blood capillaries, and increase their permeability.
• neutral proteases
• eosinophil chemotactic factor of anaphylaxis (ECF-A).
Mast cells also release leukotriens, but these substances are not stored in the cell. They are synthesized from membrane phospholipids and immediately released upon appropriate stimulation.
Mast cells originate from HSC in the bone marrow. Although they are, in many respects, similar to basophilic leukocytes, they have a separate precursor cell and are not the basophils found in connective tissue. Likewise, basophils are not circulating mast cells.
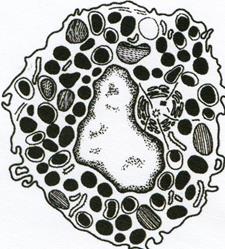 Fig. 7. MAST CELL
Fig. 7. MAST CELL
Functions:
• regulation of permeability of intercellular matrix and blood vessel wall (by slow releasing of stored substances).
• participation in the first stage of acute inflammatory responses.
• the main role in immunologic allergic reactions (by massive degranulation).
The surface of mast cells contains specific receptors for IgE, a type of immunoglobulins produced by plasma cells. Most IgE molecules are fixed on the surface of mast cells and blood basophils; very few remain in the plasma.
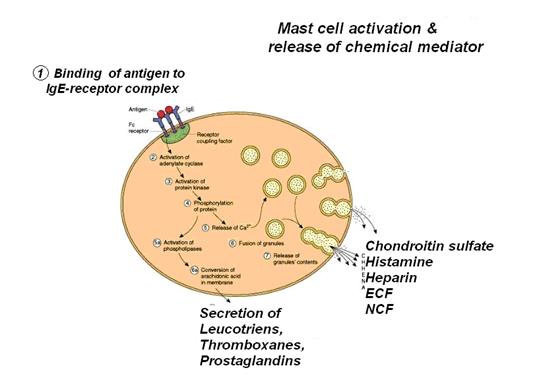
Release of the chemical mediators stored in mast cells promotes the allergic reactions known as immediate hypersensitivity reactions because they occur within a few minutes after penetration by antigen of an individual previously sensitized to the same or a very similar antigen. There are many examples of immediate hypersensitivity reaction; a dramatic one is anaphylactic shock, a potentially fatal condition.
PLASMA CELLS. Plasma cells are generated by activated B-lymphocytes. Plasma cells are large, ovoid cells that have a basophilic cytoplasm owing to their richness in RER The juxtanuclear Golgi complex and the centrioles occupy a region that appears pale in regular histological preparations. The nucleus of the plasma cell is spherical and eccentrically placed, containing compact, coarse heterochromatin alternating with lighter areas of approximately equal size. Thus, the nucleus of a plasma cell is commonly described as having a clock-face (or cartwheel) appearance.
Дата добавления: 2015-10-31; просмотров: 208 | Нарушение авторских прав
| <== предыдущая страница | | | следующая страница ==> |
| Fig.2. Structure of Proteoglycan | | | TYPES OF CONNECTIVE TISSUE PROPER |