
|
Читайте также: |
Interventional radiology
Interventional radiology (abbreviated IR or VIR for Vascular and Interventional Radiology, also referred to as Surgical Radiology) is a medical sub-specialty of radiology which utilizes minimally-invasive image-guided procedures to diagnose and treat diseases in nearly every organ system. The concept behind interventional radiology is to diagnose and treat patients using the least invasive techniques currently available in order to minimize risk to the patient and improve health outcomes.
As the inventors of angioplasty and the catheter-delivered stent, interventional radiologists pioneered modern minimally-invasive medicine. Using X-rays, CT, ultrasound, MRI, and other imaging modalities, interventional radiologists obtain images which are then used to direct interventional instruments throughout the body. These procedures are usually performed using needles and narrow tubes called catheters, rather than by making large incisions into the body as in traditional surgery.
Many conditions that once required surgery can now be treated non-surgically by interventional radiologists. By minimizing the physical trauma to the patient, peripheral interventions can reduce infection rates and recovery time, as well as shorten hospital stays.
Endovascular surgery
Endovascular surgery is a form of minimally invasive surgery that was designed to access many regions of the body via major blood vessels. Endovascular techniques were originally pioneered for diagnostic purposes by radiologists. Basic techniques involve the introduction of a catheter percutaneously into a large blood vessel (Seldinger technique). Typically the blood vessel chosen is the femoral artery or a vein found near the groin. Access to the femoral artery for example, is required for coronary, carotid, and cerebral angiographic procedures. The catheter is injected with a radio-opaque dye that can be seen on live X-ray or fluoroscopy. As the dye courses through the blood vessels, characteristic images are seen by experienced viewers and can assist in the diagnosis of diseases such as atherosclerosis, vascular trauma, or aneurysms.
In recent years, however, the development of intravascular balloons, stents and coils have allowed for new therapies as alternatives to traditional surgeries such as Coronary artery bypass surgery (CABG), carotid endarterectomy and aneurysm clipping. Stents and coils are composed of fine wire materials such as platinum, that can be inserted through a thin catheter and expanded into a predetermined shape once they are guided into place.
Endovascular surgery is performed by radiologists, neurologists, neurosurgeons, cardiologists, and vascular surgeons. The field is rapidly growing as its minimally invasive techniques offer an immediate advantage over more traditional, yet highly invasive surgeries.
Angiography or arteriography is a medical imaging technique used to visualize the inside, or lumen, of blood vessels and organs of the body, with particular interest in the arteries, veins and the heart chambers. This is traditionally done by injecting a radio-opaque contrast agent into the blood vessel and imaging using X-ray based techniques such as fluoroscopy. The word itself comes from the Greek words angeion, "vessel", and graphein, "to write" or "record". The film or image of the blood vessels is called an angiograph, or more commonly, an angiogram. Though the word itself can describe both an arteriogram and a venogram, in its everyday usage, the terms angiogram and arteriogram are often used synonymously, whereas the term venogram is used more precisely.
The term angiography is strictly defined as based on projectional radiography; however, the term has been applied to newer vascular imaging techniques such as CT angiography and MR angiography. The term isotope angiography has also been used, although this more correctly is referred to as isotope perfusion scanning.
The Seldinger technique is a medical procedure to obtain safe access to blood vessels and other hollow organs. It is named after Dr. Sven-Ivar Seldinger (1921-1998), a Swedish radiologist from Mora, Dalarna County, who introduced the procedure in 1953. The desired vessel or cavity is punctured with a sharp hollow needle called a trocar, with ultrasound guidance if necessary. A round-tipped guidewire is then advanced through the lumen of the trocar, and the trocar is withdrawn. A "sheath" or blunt cannula can now be passed over the guidewire into the cavity or vessel. Alternatively, drainage tubes are passed over the guidewire (as in chest drains or nephrostomies). After passing a sheath or tube, the guidewire is withdrawn. A sheath can be used to introduce catheters or other devices to perform endoluminal (inside the hollow organ) procedures, such as angioplasty. Fluoroscopy may be used to confirm the position of the catheter and to manoeuvre it to the desired location. Injection of radiocontrast may be used to visualize organs. Interventional procedures, such as thermoablation, angioplasty, embolisation or biopsy, may be performed.
Vascular acceses
Central venous catheter - in medicine, a central venous catheter ("central line", "CVC", "central venous line" or "central venous access catheter") is a catheter placed into a large vein in the neck (internal jugular vein), chest (subclavian vein or axillary vein) or groin (femoral vein). It is used to administer medication or fluids, obtain blood tests (specifically the "mixed venous oxygen saturation"), and directly obtain cardiovascular measurements such as the central venous pressure.
Femoral artery cannulation
Catheter-over-wire technique. The technique for femoral artery cannulation is the Seldinger technique, also known as catheter-over-wire. Prepare and anesthetize the skin, locate the vessel, and insert the needle as described above in the catheter-over-needle technique. Seldinger technique. Puncture of femoral artery with an 18-ga, 3-in hollow introducer needle (note 45-degree insertion angle). Once the needle is in the artery, use a guidewire insertion adapter to advance the guidewire through the lumen of the needle. Ensure that the guidewire passes easily, without resistance. Guidewire being inserted into the femoral artery lumen. After the guidewire has been advanced to within several centimeters of the end of the needle, remove the needle over the wire, taking care never to let go of the wire. Make a small nick in the skin at the site of the guidewire to facilitate passage of the catheter through the skin. A 2-mm incision is made next to the guidewire with a No. 11 scalpel blade. Make sure that the wire fits tightly into the end of the catheter so the catheter will enter the arterial lumen smoothly (this may be problematic, especially in patients with synthetic femoral grafts and in patients with advanced atherosclerosis). Advance the catheter over the guidewire and into the vessel.
Insertion of 20-ga, 5-in catheter over the guidewire into the femoral artery.
Remove the guidewire, leaving the catheter in place. Successful artery cannulation is confirmed by pulsatile blood flow from the catheter when the wire is removed.
Apply a sterile dressing with the date of placement over the catheter.
Haemostasis
Haemostasis is an important practical matter. Complications from diagnostic cardiac catheterization are rare, but if they happen, those related to haemostasis are the most common ones. Haemostasis may be difficult if the patient is obese, if there is high blood pressure (always try to regulate the blood pressure prior to sheath removal), or if clotting
time is prolonged. In order to facilitate the haemostasis process, haemostatic devices have been developed, such as: collagen plugs, external pressure devices, vascular clips, external C clamps, topical haemostatic accelerators etc.
Radiocontrast agents
Radiocontrast agents are a type of medical contrast medium used to improve the visibility of internal bodily structures in X-ray based imaging techniques such as computed tomography (CT) and radiography (commonly known as X-ray imaging). Radiocontrast agents are typically iodine or barium compounds.
Iodinated (intravascular)
Example of iodine based contrast in cerebral angiography
Iodine-based contrast media are usually classified as ionic or non-ionic. Both types are used most commonly in radiology due to their relatively harmless interaction with the body and its solubility. Contrast media are primarily used to visualize vessels and changes in tissues on radiography and CT. Contrast media can also be used for tests of the urinary tract, uterus and fallopian tubes. It may cause the patient to feel as if he or she has urinated on him- or herself. It also puts a metallic taste in the mouth of the patient.
Modern intravenous contrast agents are typically based on iodine. This may be bound either in an organic (non-ionic) compound or an ionic compound. Ionic agents were developed first and are still in widespread use depending on the requirements but may result in additional complications. Organic agents which covalently bind the iodine have fewer side effects as they do not dissociate into component molecules. Many of the side effects are due to the hyperosmolar solution being injected. i.e. they deliver more iodine atoms per molecule. The more iodine, the more "dense" the X-ray effect.
There are many different molecules. Some examples of organic iodine molecules are iohexol, iodixanol and ioversol. Iodine based contrast media are water soluble. These contrast agents are sold as clear colorless water solutions, the concentration is usually expressed as mg I/ml. Modern iodinated contrast agents can be used almost anywhere in the body. Most often they are used intravenously, but for various purposes they can also be used intraarterially, intrathecally (as in diskography of the spine) and intraabdominally – just about any body cavity or potential space.
Iodine contrast agents are used for the following: Angiography (arterial investigations); venography (venous investigations); VCUG (voiding cystourethrography); HSG (hysterosalpinogram); IVU (intravenous urography)
Commonly used iodinated contrast agents
Compound Name Type Iodine content Osmolality
Non-ionic Iopamidol (Isovue 370) Monomer 370 mgI/ml 796 Low
Non-ionic Iohexol (Omnipaque 350) Monomer 350 mgI/ml 884 Low
Non-ionic Ioxilan (Oxilan 350) Monomer 350 mgI/ml 695 Low
Non-ionic Iopromide (Ultravist 370) Monomer 370 mgI/ml 774 Low
Non-ionic Iodixanol (Visipaque 320) Dimer 320 mgI/ml 290 Low
Vascular Access Site Complications
Major Coronary Complications of PCI: Abrupt vessel closure; Coronary artery dissection; Thrombosis; Spasm; Air embolism; Side-branch occlusion; Distal macroembolization; No-reflow phenomenon; Aortic dissection; Coronary perforation.
Vascular access for PCI can be gained through the transfemoral, transradial or transbrachial techniques. Transbrachial access is rarely used nowadays due to the potential catastrophic complication of upper limb loss due to ischaemia. Transfemoral access is the most routinely used due to its technical simplicity, but transradial access is gaining popularity due to its better complication profile. A recent meta-analysis shows that transradial access had less entry site complications but a lower rate of procedural success due to its higher technical requirements.
The incidence of femoral vascular complications after PCI is reported to be around 2–6% (11). Transfemoral access site complications include haematoma, pseudo-aneurysm, arterio-venous (AV) fistula formation, lower limb ischaemia, femoral artery infection and retroperitoneal bleeding. Mild bruises and small haematomas are common and do not require specific investigation or treatment. A large or enlarging lump suggests either haematoma formation or pseudo-aneurysm formation and should be investigated with vascular ultrasound imaging.
Retroperitoneal bleeding results from a high needle puncture above the inguinal ligament, where blood can enter the retroperitoneum and cause abdominal or back pain without any obvious haematoma formation in the groin. Severe back or loin pain after cardiac catheterization should alert the clinician to this possibility. It can also cause severe blood loss in the absence of pain. The incidence of retroperitoneal bleeding after PCI is reported to be <0.5%.
Radial artery access is in general more comfortable for the patient and carries a much lower risk of haematoma, pseudo-aneurysm or AV fistula formation. Loss of the radial pulse can sometimes occur, but this does not cause hand ischaemia if adequate collateral circulation from the ulnar artery could be demonstrated with Allen's test before the procedure
Contrast-Induced Nephropathy. Contrast-induced nephropathy has become a significant source of hospital morbidity and mortality with the ever-increasing use of iodinated contrast media in diagnostic imaging and interventional procedures such as angiography in high-risk patients. It is the third most common cause of hospital-acquired acute renal failure, after surgery and hypotension.
The severity or degree of stenosis
Arterial stenosis or occlusion
Cause and effect. Arterial stenosis or occlusion is commonly caused by atherosclerosis, but can occur acutely as a result of emboli or trauma. Stenosis or occlusion produces symptoms related to the organ which is supplied by the artery: e.g. lower limb — claudication, rest pain and gangrene; brain — transient ischaemic attacks and hemiplegia; myocardium — angina and myocardial infarction; kidney — hypertension or infarction; intestine —abdominal pain and infarction. The severity of the symptoms is related to the size of the vessel occluded and the alternative routes (collaterals) available.
The severity or degree of stenosis is measured in the cardiac cath lab by comparing the area of narrowing to an adjacent normal segment, and as a percentage reduction and calculated in the projection which demonstrates the most severe narrowing.
The diagram below show 8 tubes that represent coronary arteries with either eccentric (E) or concentric (C) stenosis of varying severity. For example A has an eccentric stenosis. The black area within the red tube is equivalent to a stenosis that compromises 20% of the lumen of the artery. In other words, the lesion diameter is 20% of the normal vessel diameter. On the other extreme, tube G shows that the stenosis is concentric and occupies nearly 95% of the lumen (as compared to the adjacent normal artery. The other tubes represent other degrees of stenosis.
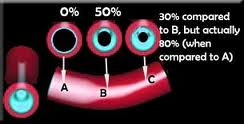
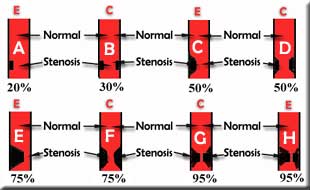
The x-ray tube is rotated around the patient (side-to-side, and also towards and away from the head), as shown below. By taking pictures from different angles, the cardiologist can inspect a stenotic lesion from several points of view. This increases the accuracy of assessing the clinical importance and severity of a blockage. It also helps determine the patients candidacy for angioplasty, stinting, surgery, medical treatment, etc. and in the selection of the device and its diameter and length (in the case of a stent).
Left caudal view (LAO-caudal, or "spider" view) is excellent for evaluation of the LMCA and its bifurcation into the LAD and CX, or trifurcation into the LAD, CX and intermediate branch if it exists.
Left cranial (LAO-cranial) view is very good for showing the ostium of the LMCA, but considerably forshortens the proximal half of the LAD. It is convenient for separating the diagonals and the septals from the LAD, though, and can be used to guide the guidewire into and from these branches during interventions. The CX and its high-originating
branches are not appreciated well in this projection, but if the CX is dominant, this projection can be useful to depict the very distal parts of the CX.
Right cranial (RAO-cranial) projection is the most useful if it is performed with increased cranial angulation of 30, or in some cases even more. This projection shows nicely the mid part of the LAD with the take-offs of diagonal branches and can in most instances be very useful for treating bifurcation lesions within the LAD + diagonals.
Дата добавления: 2015-10-26; просмотров: 192 | Нарушение авторских прав
| <== предыдущая страница | | | следующая страница ==> |
| Упражнение 3. Исследование влияние начальных условий на характер светового отклика инжекционного лазера в режиме импульсной модуляции излучения. | | | Endovascular treatment of abdominal ischemic syndrome |