
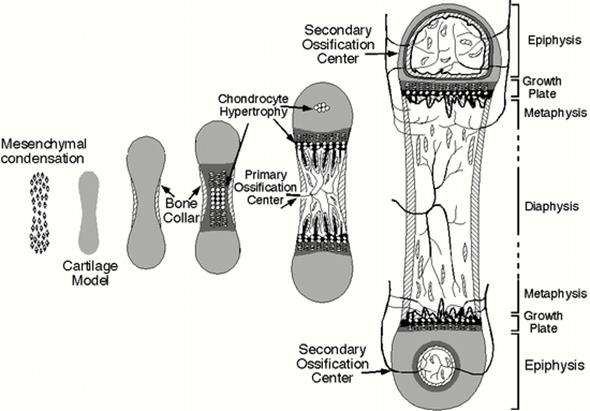
Endochondral ossification takes place within a piece of hyaline cartilage whose shape resembles a small version or model of the bone to be formed. This type of ossification is principally responsible for the formation of short and long bones.
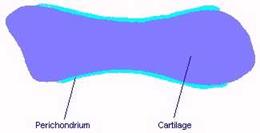
· Chondroblasts form a hyaline cartilage model of the future bone. Once surrounded by cartilage matrix they change into chondrocytes. Perichondrium is continuous with the joint capsule. Blood vessels supply the perichondrium
· Osteoprogenitor cells from the perichondrium change to osteoblasts. Osteoblasts produce a woven bone collar surrounded by periosteum (perichondral bone). Chondrocytes start to hypertrophy in the diaphysis. The matrix between them is mineralized forming calcified cartilage. Chondrocytes trapped in their calcified tombs die leaving lacunae with thin calcified matrix walls.

• Blood vessels invade lacunae in the calcified cartilage. Osteoprogenitor cells travel into the calcified cartilage via the connective tissue of blood vessels.

• The osteoprogenitor cells give rise to osteoblasts, which cover the cartilaginous septa with bone matrix. The septa of calcified cartilage tissue thus serve as supports for the beginning of ossification. Osteoblasts produce bone trabeculae (endochondral bone) in diaphysis forming spongy bone.
This part of the future bone is called the primary ossification center.
• Bone collar thickens and lengthens. Medullary cavity forms when osteoclasts remove bone from the diaphysis. Bone marrow is produced in the newly formed medullary cavity.

· At later stages in embryonic development, a secondary ossification center arises at the center of each epiphysis. The function of these centers is similar to that of the primary center, but their growth is radial instead of longitudinal. Furthermore, since the articular cartilage has no perichondrium, there is no equivalent of a bone collar formed here.

• When the bone tissue that originated at the secondary centers occupies the epiphysis, cartilage remains restricted to 2 places: articular cartilage, which persists throughout adult life and does not contribute to bone formation; and epiphyseal cartilage, or the epiphyseal growth plate, which connects epiphysis to diaphysis.
As the cartilage of the epiphyseal plate grows, it is replaced continuously by newly formed bone matrix. No further longitudinal growth of the bone takes place after the growth of the epiphyseal plate ceases.
Epiphyseal plate is divided into 5 zones, starting from the epiphyseal side of cartilage (Fig.34):

•
•
•
• The resting zone consists of hyaline cartilage without morphologic changes in the cells;
• In the proliferative zone, chondrocytes divide rapidly and forms columns of stacked cells parallel to the long axis of the bone;
• The hypertrophic zone contains large chondrocytes whose cytoplasm has accumulated glycogen. The resorbed matrix is reduced to thin septa between the chondrocytes.
• Simultaneous with the death of chondrocytes occurring in the calcified cartilage zone, the thin septa of cartilage matrix become calcified by the deposit of hydroxyapatite.
• In the ossification zone, endochondral bone tissue appears. Blood capillaries and osteoprogenitor cells invade the cavities left by the chondrocytes. The osteoprogenitor cells form osteoblasts, which in turn form a discontinuous layer over the septa of calcified cartilage matrix. The bone matrix calcifies, and some osteoblasts are transformed into osteocytes. In this way, bone spicules are formed with a central area of calcified cartilage and a superficial layer of primary bone tissue.
The rates of these 2 opposing events (proliferation and destruction) are approximately equal, and thus the epiphyseal plate does not change thickness. Instead, it is displaced away from the middle of the diaphysis, resulting in growth in length of the bone.
Plasticity. In spite of its hardness, bone is capable of remodeling its internal structure according to the different stresses to which it is subjected. Bone responds to injury by rapid healing. Bones are continually being modified, reshaped, remodeled.
Дата добавления: 2015-10-31; просмотров: 118 | Нарушение авторских прав
| <== предыдущая страница | | | следующая страница ==> |
| SECONDARY (LAMELLAR) BONE | | | Молярная концентрация растворенного вещества или молярность раствора. |